© 2016, BSM Consulting
7
Basics of Glaucoma
treated early, most babies with congenital glaucoma maintain some degree of sight, with some
experiencing excellent vision.
Juvenile-onset primary open-angle glaucoma has some features of both congenital glaucoma and adult-
onset primary open-angle glaucoma. Some cases respond well to medications, and others require
surgery.
DIAGNOSTIC TESTING IN GLAUCOMA
The diagnosis of glaucoma is extremely complex, requiring the eye physician to use a battery of tests,
clinical findings, and patient history to determine a glaucoma diagnosis and to check for progression
(worsening). The following sections will describe the testing physicians require to make this diagnosis.
DIAGNOSTIC TESTING: GLAUCOMA
Tonometry:
measures intraocular pressure
Ophthalmoscopy:
evaluates the optic nerve
SCODI
(scanning computerized diagnostic imaging): evaluates
the optic nerve head and monitors changes
Gonioscopy:
evaluates the angle structure
Pachymetry:
measures thickness of the cornea
Visual Fields:
evaluates peripheral field of vision
Clinical Measurement of Intraocular Pressure
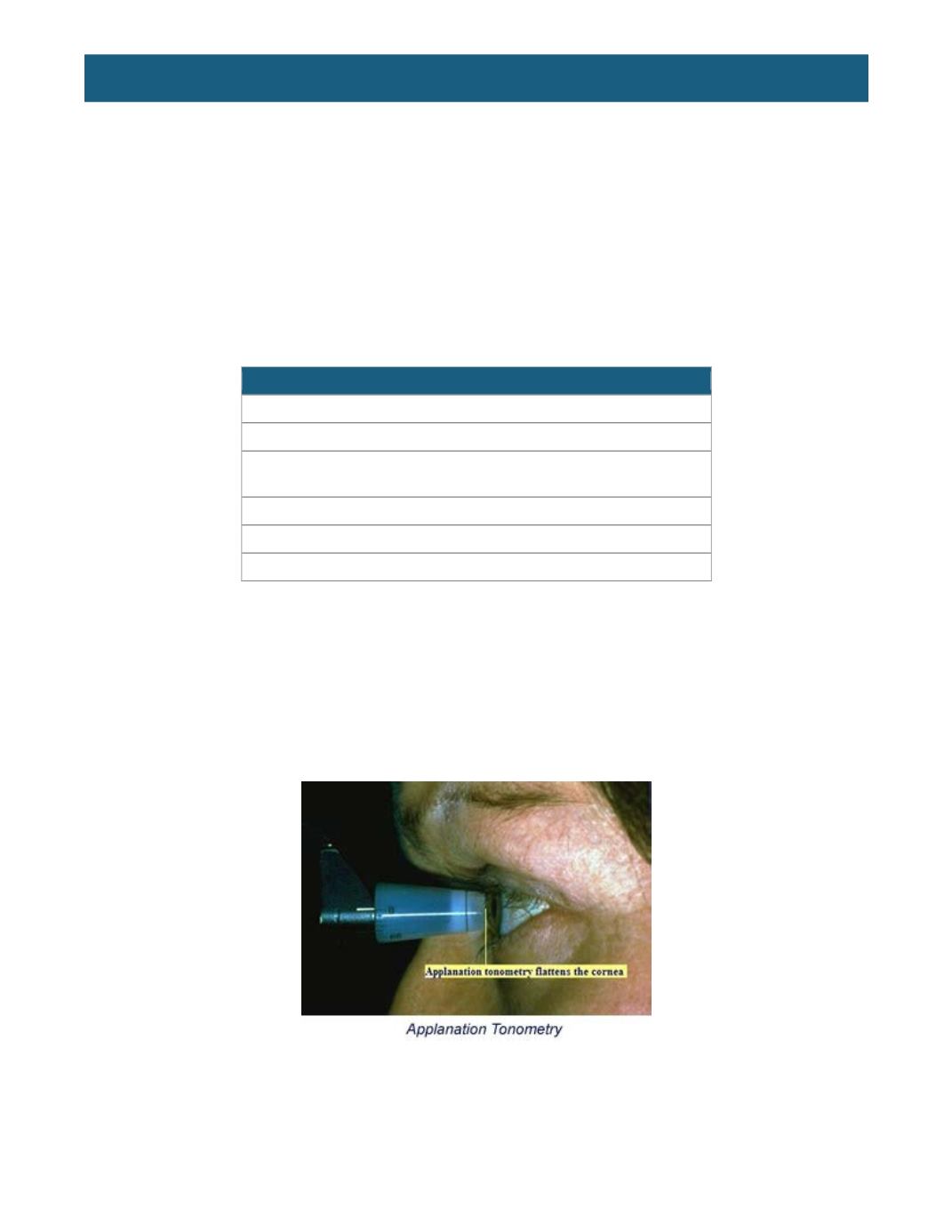
Measurement of IOP in a clinical setting requires a force that indents or flattens the eye. Applanation
tonometry is based on the principle that the pressure inside a thin-walled sphere equals the force
necessary to flatten its surface, divided by the area of the flattening. The Goldmann applanation
tonometer measures the force necessary to flatten an area of the cornea of 3.06 millimeters diameter,
where the resistance of the cornea to flattening is counterbalanced by the capillary attraction of the tear
film meniscus for the tonometer head.
Furthermore, the IOP in millimeters of mercury equals the flattening force (in grams) multiplied by 10. A
split-image prism allows the examiner to determine the flattened area with great accuracy. Fluorescein in
the tear film is used to outline the area of flattening. The semicircles, called mires, move with the ocular
pulse, and the endpoint is reached when the inner edges of the semicircles touch each other at the
midpoint of their excursion. The dial is read, then multiplied by 10 to produce the IOP reading in
millimeters of mercury.
















