© 2016, BSM Consulting
2
Basics of Glaucoma
When a patient with elevated pressure is thoroughly evaluated and found to have no evidence of optic
nerve damage or visual field loss, the physician may diagnose ocular hypertension, or glaucoma. Patients
in this category are usually those with pressures in the low- to mid-20s, but occasionally higher. These
patients either may develop glaucomatous damage over the next months to years, or may never develop
damage at all. Eye physicians may decide to treat an ocular hypertension patient on the basis of age,
medical history, family history of glaucoma, or condition of the fellow eye, rather than wait for evidence of
optic nerve damage or visual field changes.
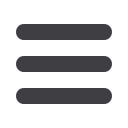
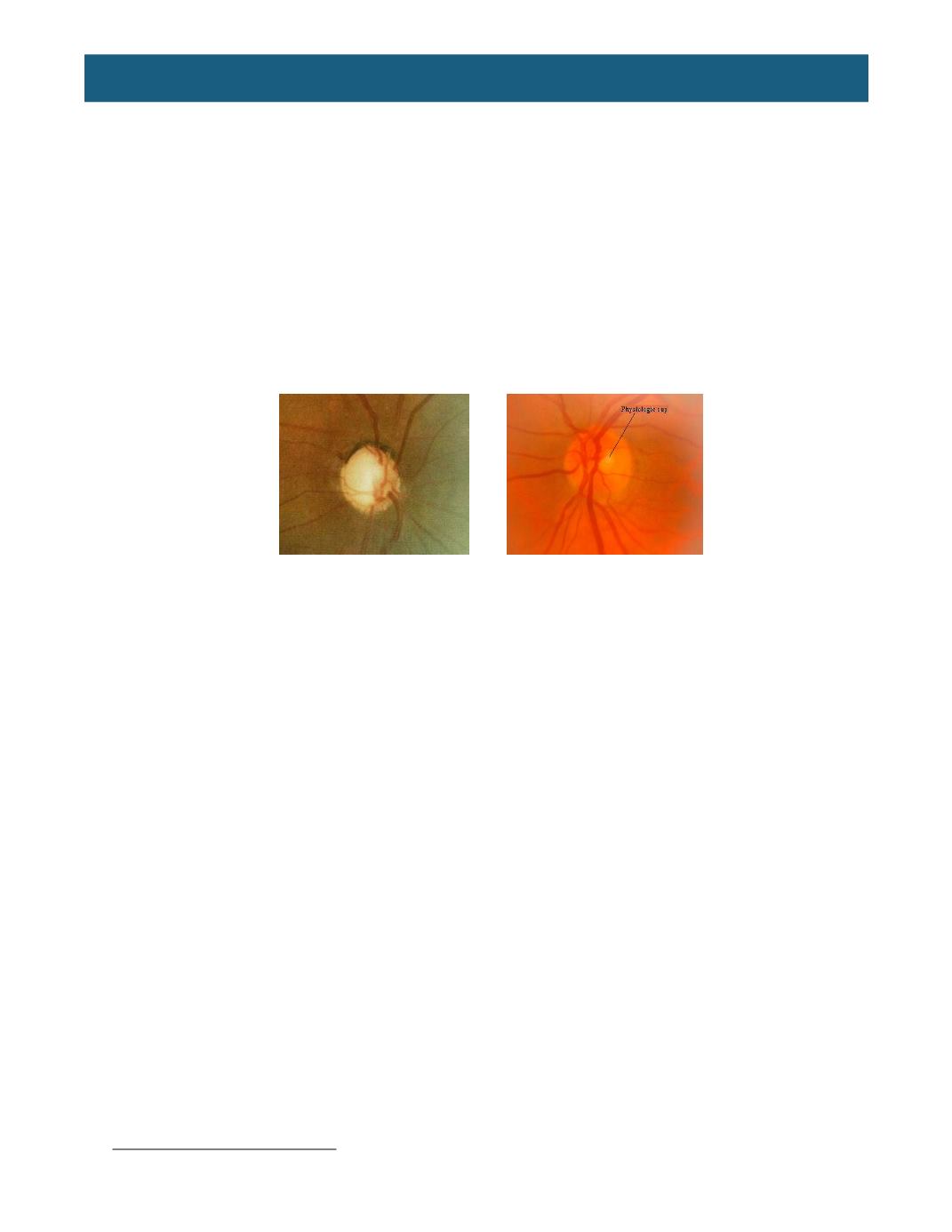
Additionally, doctors may suspect glaucoma if the patient’s optic nerves are either abnormal in
appearance or are not mirror images. The optic nerve is housed within the optic disc. As IOP increases
and presses on the optic nerve, the area of the “cupping” can increase in size. The amount of “cupping” is
described by the cup-to-disc (CD) ratio, which ranges from 0.0 to 1.0. A larger CD describes a greater
amount of cupping of the disc, increasing the possibility of glaucomatous damage. If the patient’s optic
discs are unequal in appearance, the physician might suspect glaucoma secondary to optic nerve
asymmetry.
Abnormal Cupping Normal Cup-Disc-Ratio
Frequently, a pachymeter will measure the corneal thickness of glaucoma suspects to determine if the
cornea is thicker or thinner than average. Ocular hypertensive patients with thicker-than-normal corneas
develop glaucoma much less frequently than patients with thin, or even normal, corneas, provided that all
other factors (age, IOP level, cup size, etc.) are equal. Average corneal thickness is 0.535 to 0.565
millimeters (or 535 to 565 microns). Applanation tonometry of an unusually thin cornea can result in a
false reading that is lower than the actual IOP because the resistance of the corneal tissue is less than
expected. Additionally, a thick cornea will give a false high applanation reading because the resistance of
the corneal tissue is greater than expected. Modern thought seems to indicate the thinner-than-average
cornea might indicate a more vulnerable optic nerve.
RISK FACTORS OF GLAUCOMA
There are several demographic and health trends that have increased the number of people at risk of
glaucoma. In addition to genetic risk factors among immediate family members, according to the
Glaucoma Research Foundation,
4other risk factors include:
•
Age:
Adults older than 60 are six times more likely to develop glaucoma than their younger
counterparts. As the number of older Americans grows, so does the number of glaucoma
patients.
•
Race:
The risk of glaucoma is six to eight times greater among African-Americans than
Caucasians; Hispanics run a higher risk than people of European descent; Asians represent a
significant percentage of patients with angle-closure glaucoma.
•
Obesity and diabetes:
Diabetic patients are twice as likely to develop glaucoma as people
without the disease. As diabetes and obesity reach epidemic proportions, the number of
glaucoma cases is expected to increase, as well.
4
Glaucoma.org















