© 2016, BSM Consulting
5
Modern Glaucoma Surgery
scleral flap could scar down to its bed, preventing fluid from percolating from under the flap into the
subconjunctival bleb. Or the conjunctiva could scar down to the sclera, preventing bleb formation. This is
undesirable as it would cause the surgery to fail. To prevent this scarring, we can apply one of two
chemicals to the ocular surface during the procedure. These chemicals are 5-fluorouracil (5-FU) and
mitomycin-C (MMC) and are used as systemic chemotherapy agents for a variety of gastrointestinal
cancers. They prevent cell division, which is useful in getting cancer cells to stop growing and is also
useful in preventing the cells involved in scarring from proliferating at the glaucoma surgery site. MMC is
typically delivered to the eye soaked into a small sponge and placed between the sclera and the
conjunctiva for 1–5 minutes before or immediately after dissection of the scleral flap but before entering
the eye. 5-FU is usually administered in the same fashion and can also be injected subconjunctivally for
the first few postoperative days as needed to augment the intraoperative dose. While these agents are
very good at preventing scar formation, they can also prevent normal healing of the surgery. The
conjunctiva must be cut open and needs to be completely sealed back in order for the bleb not to leak.
Use of antimetabolites can slow the healing of the conjunctiva, resulting in bleb leaks, which are a risk
factor for both hypotony (because too much fluid exits the eye) and infection (because bacteria can get
into the eye through the hole in the conjunctiva and then the hole in the trabecular meshwork). Some
surgeons use one or the other of these drugs in every glaucoma surgical case. Others use them only in
patients at high risk for failure by scarring. Risk factors that might prompt the use of antimetabolites
include black race, younger patients, prior conjunctival surgery (especially a previous failed
trabeculectomy), and inflammatory or neovascular glaucoma.
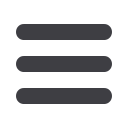
Ex-Press Mini Shunt
As stated previously, one way a trabeculectomy can fail is for the hole in the trabecular meshwork to heal
shut. The Ex-PRESS mini shunt is a small hollow tube that is inserted into this hole and keeps the hole
propped open so it cannot heal shut (
Figure 2
). Additionally, the device has a standard internal diameter
so that aqueous fluid flow out of the eye is somewhat regulated with the goal of reducing the risk of
postoperative hypotony.
This surgical procedure is almost identical to trabeculectomy. After the scleral flap is fashioned, a needle
(the same diameter as the Ex-PRESS device) is stabbed through the bed of the scleral flap into the
anterior chamber. The needle is withdrawn and the Ex-PRESS device is inserted through the hole. It has
a spur on the end that goes into the eye, and when the device is passed far enough into the eye, the spur
pops into the eye and serves as a hook to prevent the device from exiting of the eye. It has a flange on
the outer end to prevent it from going too far into the eye. Once in position, the flap is sutured and the
conjunctiva closed. Iridotomy is not performed because the eye is never opened more than the diameter
of the needle stab so it cannot make contact with the iris. This device reduces the risk of failure from the
hole healing shut, but failure from scarring of the flap to its bed or of the conjunctiva to the sclera are still
possible, so antimetabolites are typically used as with trabeculectomy.
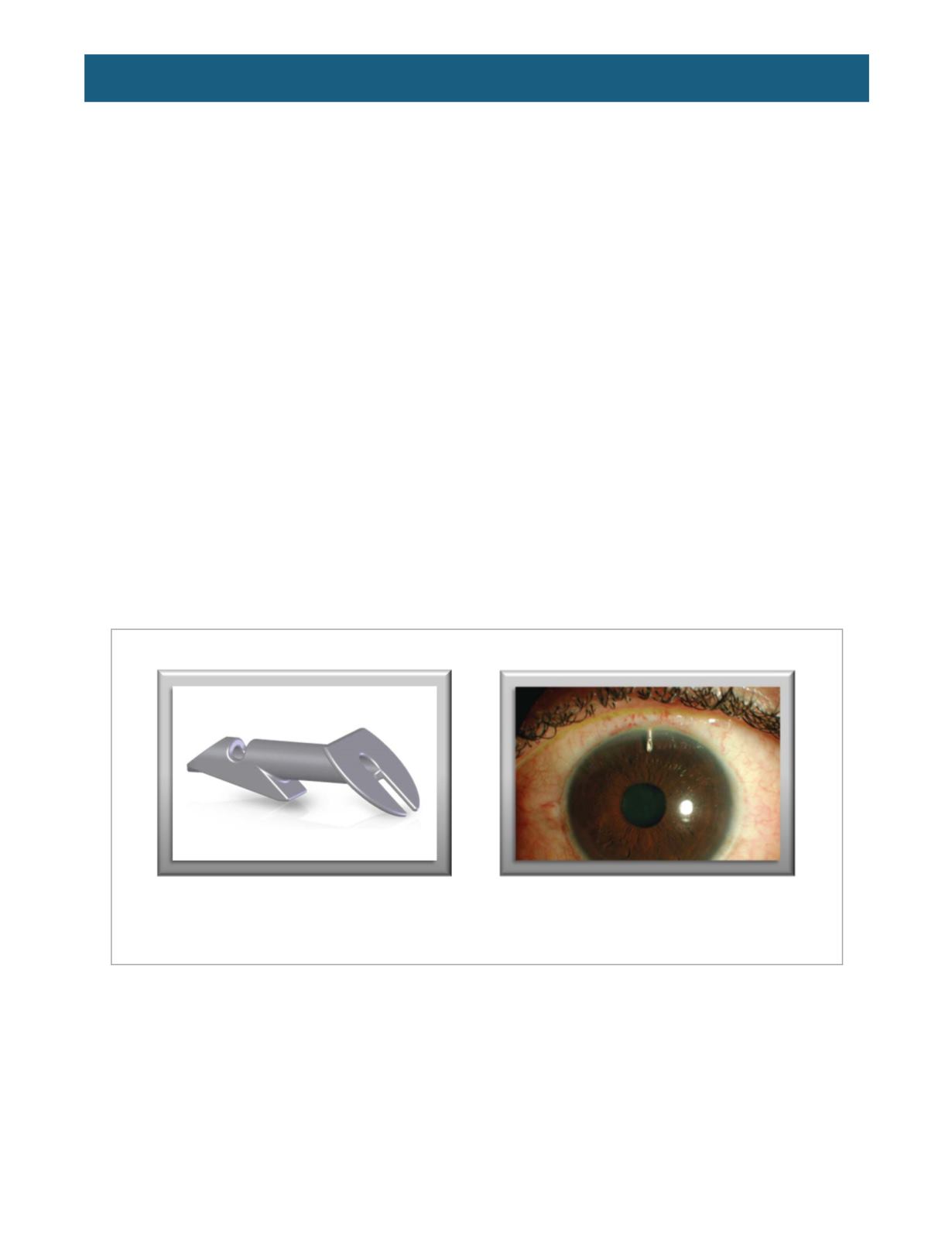
Figure 2.
The Ex-PRESS mini shunt.
Above left,
the device itself.
Above right
, the device after implantation.
(From
http://www.alconsurgical.com/glaucoma-filtration-device-specifications.aspxand
http://www.revophth.com/content/d/glaucoma_management/i/1296/c/24959/)














