© 2016, BSM Consulting
2
Modern Glaucoma Surgery
likely that most patients will require multiple medications to achieve adequate IOP control. Patients whose
glaucoma cannot be controlled with medications—or who cannot faithfully use medications or prefer not
to use them—can undergo a laser procedure called trabeculoplasty. This procedure effectively lowers
IOP for many patients by unclogging the drain, although its effect tends to wear off over time as the drain
reclogs, requiring the need for a repeat trabeculoplasty one or more years later
. 11For difficult cases of
glaucoma that do not respond well to medical or laser therapy, surgical intervention may be necessary.
The progression from medications to laser to surgery
reflects the increasing risk with each progressive
step. While surgery can lower IOP more effectively
than medications or laser therapy, it also has more
serious potential complications. Therefore, the
decision to proceed to glaucoma surgery should be
based on a careful assessment of the patient and a
risk/benefit analysis that justifies the potential risks of
surgery in order to prevent vision loss. Several
different events can justify the need for glaucoma
surgery (
Table 1
). One common reason that
glaucoma surgery is necessary is that the IOP
remains above the target IOP despite the use of all
tolerated medications and the prior application of laser therapy. In this case, every effort should be made
to determine whether the patient is truly using the medications as prescribed. In some instances, poor
adherence to therapy can be identified and addressed and surgery avoided. Another common justification
for surgery is the progression of damage to the optic nerve head or the visual field. Particularly in the
case of visual field progression, any new change should be confirmed on at least one additional visual
field test before proceeding with surgery, as false-positive progression on visual field testing is not
uncommo
n. 12A less common reason for glaucoma surgery is intolerance to topical medications, which
can be related to an allergy to the preservatives in the medications. Similarly, some patients cannot self-
dose their medications due to physical limitations (e.g., tremor or arthritis) or cognitive limitations (e.g.,
dementia).
PRINCIPLES OF GLAUCOMA SURGERY
The goal of all glaucoma surgical procedures (
Table 2
) is to lower IOP. The vast majority of glaucoma
surgeries lower IOP by increasing outflow, generally by means of bypassing the clogged trabecular
meshwork.
The most commonly performed procedures involve
creation of a full-thickness trans-scleral bypass,
including trabeculectomy, the Ex-Press mini shunt,
and the tube-shunt. These procedures allow
aqueous fluid to drain into the subconjunctival
space, where it is eventually reabsorbed into the
bloodstream through the conjunctival blood vessels.
All three of these procedures require the creation of
a permanent reservoir of aqueous under the
conjunctiva, called a bleb.
It is also possible to bypass just the trabecular
meshwork without involving other structures of the
eye wall, as is the case with trabecular ablation
using the TrabecTome and stenting the meshwork
using the iStent. These procedures facilitate
aqueous flowing from the anterior chamber directly
into Schlemm’s canal, and thus do not result in the
formation of a bleb.
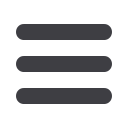
TABLE 1
Events Justifying Glaucoma Surgery in Patients
Treated With Medical ± Laser Therapy
•
IOP determined to be too high
•
Progression of the visual field
•
Progression of the optic nerve
•
Intolerance to glaucoma medications
•
Inability to self-dose glaucoma medications
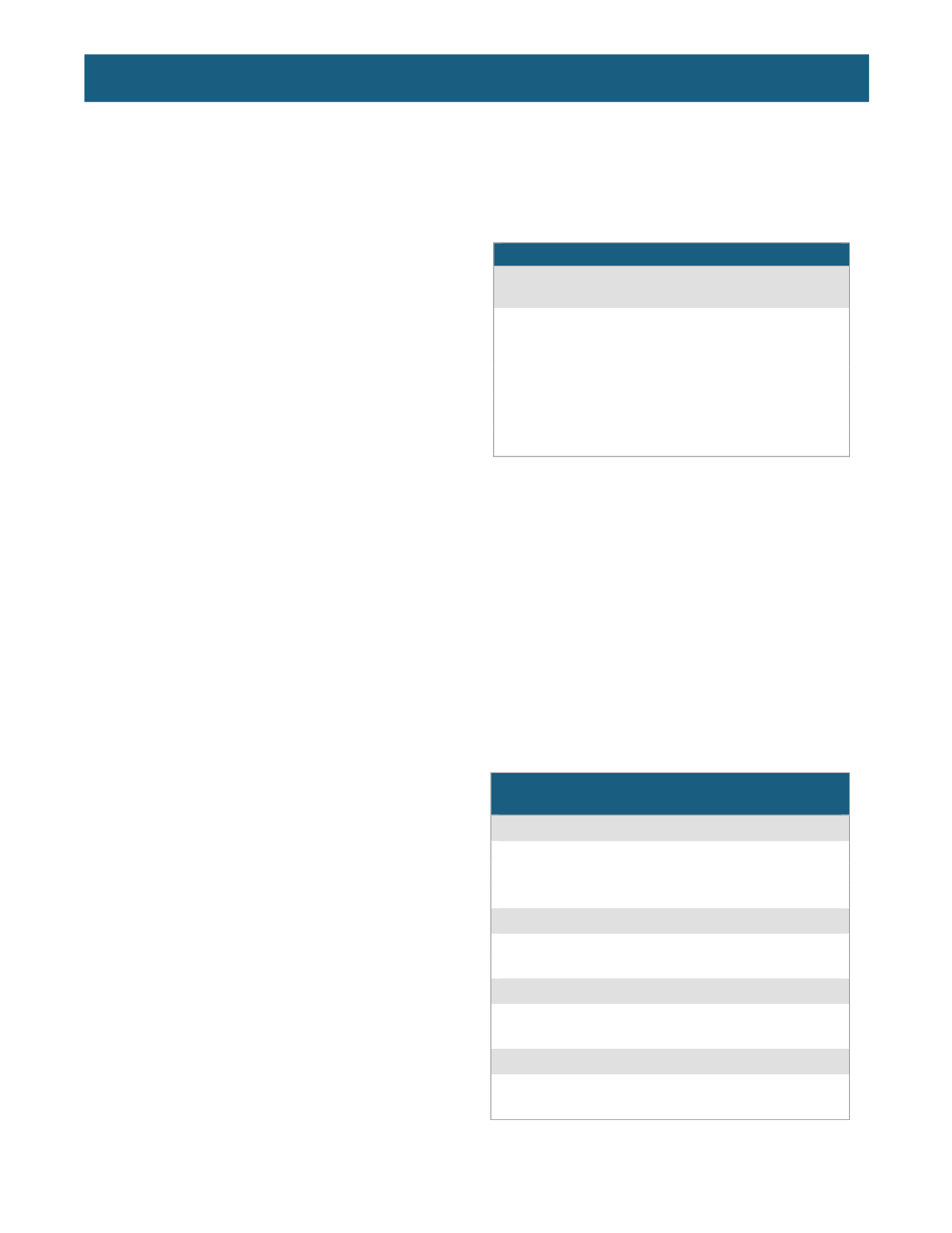
TABLE 2
GLAUCOMA SURGICAL PROCEDURES
Bleb-based procedures
•
Trabeculectomy
•
Ex-Press
•
Tube-shunt
Trabecular bypass procedures
•
Trabecular ablation (TrabecTome)
•
Trabecular stenting (iStent)
Other outflow procedures
•
Deep sclerectomy ± viscocanalostomy
•
Canaloplasty
Cilioablation procedures
•
Laser
•
Cryotherapy














