© 2016, BSM Consulting
14
Modern Glaucoma Surgery
resistance to aqueous outflow. In this latter case, there is usually a large bleb. All of the
approaches described for bleb leaks can also be applied to overfiltering blebs, including the
possibility of surgical revision. If the anterior chamber is shallow and the IOP is high, there is
cause to suspect aqueous misdirection syndrome. This occurs when aqueous flows posteriorly
into the vitreous cavity, pushing the vitreous and lens (crystalline or implant) forward, flattening
the chamber. Since aqueous is not exiting through the newly created drain, the bleb is usually low
or flat. Aqueous misdirection syndrome will often resolve with high-dose atropine therapy, may
require an Nd:YAG laser application to make a hole in the anterior vitreous to create a pathway
for aqueous to flow back forward (which can only be performed in pseudophakic or aphakic
eyes), or in more recalcitrant cases, surgical vitrectomy.
•
Shallow or flat bleb.
This can occur when there is a bleb leak (in which case IOP is usually low) or
if the surgical drainage hole is blocked, preventing aqueous from reaching the bleb (in which case
IOP is usually high). Bleb leaks are addressed previously in
Wound leaks.
Outflow obstruction in
the immediate postoperative period is usually due either to a blood clot, a fibrin clot, or too-tight
suturing of the scleral flap. All are serious risk factors for bleb failure, because if there is no
aqueous in the bleb, the conjunctiva is in direct contact with the underlying sclera and can scar
down to it, preventing future bleb formation once the obstruction is resolved. A blood clot can be
resolved by injecting tissue plasminogen activator (tPA), a potent clot-dissolving medication,
directly into the anterior chamber, although this runs the risk of a large hyphema if the vascular
defect that caused the clot has not yet healed under the clot. A fibrin clot can often be washed
away by burping the surgical site. This is performed by gently pressing a sterile instrument (such
as a scleral depressor) against the sclera (through the conjunctiva) adjacent to the edge of the
scleral flap. The goal is to transiently lower the resistance to outflow, so that a small burst of
aqueous through the surgical drain will wash the fibrin clot away. If the problem is that the flap
has been sutured too tightly, the argon laser can be used to cut one or more of the sutures
holding the flap down (again, through the conjunctiva, using a special lens designed for just this
purpose) to reduce the resistance to outflow. Some surgeons prefer using releasable sutures for
the scleral flap. These do not require cutting with a laser—they are placed in such a way that the
surgeon can grasp one externalized end at the slit lamp and pull it out, loosening the scleral flap.
If these measures fail, the scleral flap may be scarring down to its bed. In this case, the bleb may
require needling. A 30-gauge needle is inserted through the conjunctiva and advanced under the
scleral flap, then tilted slightly to elevate the flap and peel it free from the bed. The needle tip can
also be advanced through the drainage hole into the anterior chamber to clear any scar formation
in that location. This procedure is typically followed by several daily subconjunctival injections of
5-FU to minimize the risk of recurrent scarring. Needling can be performed at the slit lamp.
•
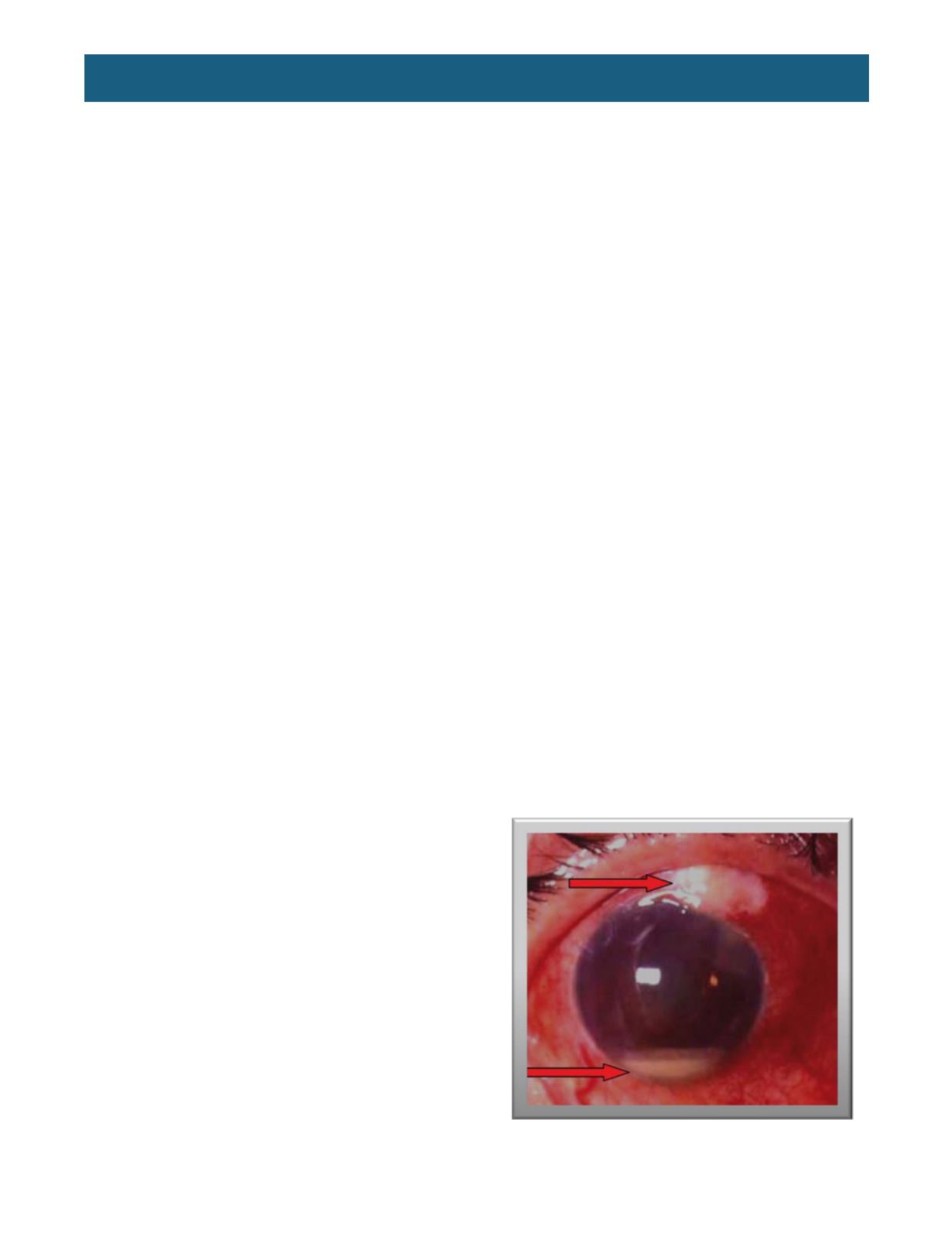
Infection.
Blebitis and/or endophthalmitis is
the worst-case scenario for bleb surgery.
Endophthalmitis due to contamination at the
time of surgery typically presents within 48
hours; blebitis/endophthalmitis related to a
bleb leak can occur any time postoperatively
as long as the bleb is functional. The patient
will present with a red, painful eye and
decreased vision. There may be visible pus
on the eye surface or in the bleb, and
examination will reveal a hypervascularized
bleb, cell and flare and possibly a hypopyon
in the anterior chamber, and possibly
inflammatory debris in the vitreous (
Figure 8
).
This is an emergency and can lead to loss of
the eye if not appropriately addressed. A
vitreous biopsy is required to culture to
identify the organism causing the infection,
followed immediately by high-potency broad-
spectrum antibiotics delivered topically,
intravitreally, and orally. It may seem tempting
to give the antibiotics before all else, but if the
Figure 8.
Blebitis/endophthalmitis with hypopyon in
the anterior chamber.
(From
http://www.ijo.in/viewimage.asp?img=IndianJOphthalmol_2011_59_7_131_73689_u15.jpg)














